Content previously published in Journal of Daoist Studies, 3, 2010.
Posted with permission from the editor of the Journal of Daoist Studies
ELENA VALUSSI, Loyola University Chicago
This article examines the following eight publications on women’s qigong techniques:
Videos
Chia, Mantak, 1998. Slaying the Red Dragon.
Lee, Daisy. n.d. Radiant Lotus: Qigong for Women.
Liu, Yafei. n.d. Nüzi qigong (Chinese/German).
Books
Chia, Mantak. 2005 [1986]. Healing Love through the Dao: Cultivating Female Sexual Energy. Destiny Books.
Davis, Deborah. 2008. Women’s Qigong for Health and Longevity: A Practical Guide for Women Forty and Over. Shambhala.
Ferraro, Dominique. 2000. Qigong for Women: Low-impact Exercises for Enhancing Energy and Toning the Body. Healing Arts Press.
Johnson, Yangling Lee. 2001. A Woman’s Qigong Guide: Empowerment through Movement, Diet and Herbs. YMAA Publication Center.
Zhang, Tinna Chunna, 2008. Earth Qigong for Women: Awaken Your Inner Healing Power. Blue Snake Books.
Female meditation techniques in China
The point of departure for this article is my research on female meditation techniques in China, also called nüdan 女丹, of female alchemy. Over the last few years, I have described the historical emergence of the nüdan tradition and its Chinese development both in my dissertation and several articles (see Valussi 2003; 2008a; 2008b; 2008c; 2009). Simply put, female alchemy is a textual tradition of Daoist meditation and physiological exercises for women, which emerged in China in the seventeenth century and developed throughout the nineteenth and twentieth centuries. It is part and parcel of the much older tradition of internal alchemy (neidan 內丹), which advocates the possibility to achieve immortality through the progressive refinement of the body, aided by meditation, breathing, visualization, and massage exercises. Unlike neidan, though, nüdan followers adapt theory, practice, and language specifically to the female body.
My research reviewed most of the historical literature available in Chinese on meditation techniques for women, as well as contemporary publications on female meditation techniques in Chinese and English. When talking about contemporary publications on the topic, while Chinese publications are mostly a contemporary rendition of historical texts, those in Western languages and especially in English reveal a vast contemporary market of healing, spiritual, and meditative techniques for women inspired by Chinese traditions. For the purposes of this paper, I chose to concentrate on American publications simply because I am more familiar with them, but I am aware that these techniques have reached Western audiences outside of the U.S., and one of the items on my list was produced in Germany (Liu Yafei video).
Historical Context
Historically, nüdan texts were produced within the Daoist tradition, mostly during sessions of spirit-writing, a form of communication between gods and the community of believers, starting in the seventeenth century. They were religious texts, guiding practitioners to immortality and ascension into heaven. This is definitely not the context in which these techniques are described, taught, and performed in the United States. Their aim, rather than complete transcendence, is health and well-being. Even though there is often, but not always, a clear spiritual component in these publications, it is seen as yet another way to help the healing process.
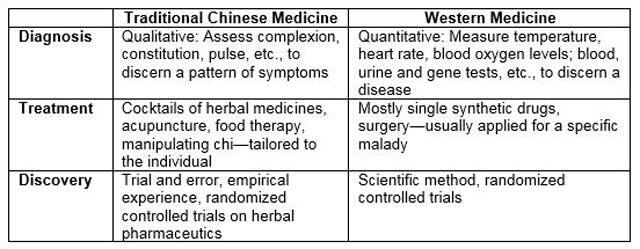
Offerings available on the American market are wide and varied. In some instances, language and techniques are quite similar to what is found in historical nüdan texts; in others the practices seem to have no link whatsoever with that tradition. Some contemporary publications have a strong focus on sexuality and its importance in the physical and spiritual well-being of practitioners: this is not present in nüdan works and generally uncommon in the neidan tradition. Yet despite the variety, I found that nüdan techniques and language are widely used and appropriated in Western publications. It is also useful to mention that most of the neidan techniques of old are now referred, both in China and in the West, as qigong, a more modern term that is less linked to a religious milieu and favors a health-scientific background.
The mysticism surrounding the techniques and the oral transmission between master and disciple of Daoist techniques, common in Daoist communities in traditional China until the late Ming dynasty, started to dissipate in the Qing when practices became available more widely to a larger market through cheap publications and open transmissions. Secrecy almost ceased in the 1930s, when inner alchemy transformed from a religious to a lay practice and its techniques became a political tool of nation strengthening. In the Republican period, intellectuals reformulated and reorganized alchemical knowledge in order to renew the Chinese heritage, which they thought needed reviving in the face of Western cultural and political onslaught as well as of the Japanese invasion. This effort was intended to help national strengthening and progress.
Under Communist rule after 1949, traditional techniques were not discarded but made even more accessible and public. Already in the 1940s Communists formulated a conscious policy for the “Liberated Areas” to make use of local medical resources within a “scientific orientation.” Mao called on modern-trained doctors to unite with traditional therapists who were closer to the people, encouraging them to “help them to reform” (Palmer 2007, 29). Accordingly traditional neidan techniques were “reformed” to meet contemporary “scientific” standards. Liu Guizhen, a local Communist cadre, who brought these practices to the Party’s attention, spearheaded this transformation from neidan to more “modern” and “scientific” practices, which eventually lead to the creation of qigong. Together with a group of other cadres, Liu “set to work on the task of extracting the method from its religious and ‘superstitious’ setting. The method was compared with techniques described in classical medical texts, its concepts and were reformulated, and its mantras ‘reformed’ (Palmer 2007, 31).
During the Cultural Revolution in the 1960s and 70s, qigong fell out of favor. It was rediscovered in the 1980s, the time of “qigong fever,” then made its way to the West both through Chinese and Western practitioners. The latter incorporated it in regimens that fit Western healing styles, some with more spiritual accents, others purely health regimens, others again with sexual overtones, and many marketed as forms of “spiritual healing”.
Much work has been done in the intersection between religion and healing; in the West the category of “spiritual healing” has widened to encompass many techniques that might at one point have been connected with specific religious traditions but that are now used in separation from their original religious context to heal a variety of ailments (see Cohen 2002-03). In the specific case of Chinese spiritual healing and qigong, too, some powerful studies have appeared, detailing the specificity of Chinese conceptions of the body and healing, as well as the political implications of the practice of qigong in China (e.g., Ots 1994; Chen 2003). There are also some studies on the transfer of knowledge to the West, notably in the field of acupuncture. Linda Barnes, in her 1998 article on the Western adoption of Chinese healing techniques and especially acupuncture, argues that “this indigenization of Chinese practices is a complex synthesis which can be described as simultaneously medical, psychotherapeutic, and religious” (1996, 1). She describes a process of acculturization that is at first uncritical, then becomes more and more inquisitive: “Initially, there was a tendency among the non-Chinese to adopt these teachings uncritically. Over time, however, they began to look for sources and methods through which to articulate questions, which, in some instances, they themselves had introduced into the Chinese practices” (1998, 415).
The process of questioning that acupuncture has undergone over the past three decades has yet to happen for qigong practices, especially those dedicated to women. Only now do critical views of some practices and the questioning of sources appear in American qigong circles. Where do the practices come from? What is the affiliation of the people who teach and write about them?
In many ways the traditional secrecy that had clouded the transmission of neidan and also qigong in China has been more accentuated with their transfer to Western practitioners. Books often describe the origins of practices as often shrouded in mystery or too ancient to be verifiable. This is entirely unnecessary. Both Chinese and Western scholars outline the historical development of neidan as well as qigong traditions, schools, and techniques (see Kohn and Wang 2009). For the modern period, especially the works of Xun Liu (2009) David Palmer (2006) and Nancy Chen (2003) trace the birth and growth of neidan and qigong during the Republican era and under Communism as a mixture of inner alchemical techniques and Western medicine. For the pre-modern period, many more monographs, articles and books are now available. At this stage Western practitioners should take these studies into consideration instead of describing the Chinese tradition as an ahistorical continuum that contains all techniques, schools, and teachers. The various presentations of women’s qigong discussed below would have greatly benefited from such consideration.
Nüzi Qigong
This DVD is by the physician and qigong teacher Liu Yafei, the daughter of Liu Guizhen, the cadre responsible for the transition from neidan to qigong. Liu Yafei works at the Beidaihe sanatorium in northern China founded by her father and teaches widely abroad, mainly in Europe, but has not yet published Western language books on her practice. In her DVD and classes she keeps the practice firmly within the realm of medicine and healing, downplaying any spiritual or religious elements. This stance is partly related to the transformation that alchemical techniques underwent during the Republican and Communist periods, and partly due to the fact that her father had been harshly criticized for his involvement in the development of qigong. The repression of the Falungong religion and various qigong forms in China today, and the limits of religious expression also play a role.
Still, there are obvious similarities in Liu’s terminology and traditional nüdan texts, starting with the cosmological positioning and defining of men and women. “Men are strong and refine their qi, women are soft and refine their blood. Women have inner soft beauty. Men are high mountains, women are flowing water.” Both practices pay specific attention to the breasts, and especially to the point between them, historically considered the starting point for female practice and the activating point for women. Both also include extensive and repeated breast massages. In addition, they pay attention to the lower abdomen, and to the Meeting Yin (huiyin) point at the perineum. All of these points are located on an extraordinary vessel (Renmai, Dumai, Chongmai, or Daimai). According to Liu, they are essential for female health because they cross the front part of the body and intersect on the abdomen. She thus applies nüdan knowledge to Chinese medical readings of the body.
Another element essential in both practices is blood. However, whereas nüdan sees blood as a pool of energy to be transformed, nüzi qigong supports its normal function. The exercises accordingly serve to regulate menstruation and female hormones, to eliminate breast problems like cysts, to help in recovery after breast cancer as well as during pregnancy and menopause, and generally to maintain and improve the blood and energy flow in the body.
Not all of nüzi qigong derives from nüdan, though. Many elements also come from neiyang gong, internal nourishing, the other form of qigong Liu teaches. Her language in all cases is eminently biomedical, speaking of different health problems and of how this practice can help solve them. The questions asked by the practitioners during classes are equally focused on health and healing. No mention is made of a spiritual or religious dimension of this practice.
Radiant Lotus
Daisy Lee is a qigong instructor certified by the National Qigong Association. The DVD, after showing a class of her students performing a series of exercises specific to female health, contains an interview on her practice. Lee notes that Radiant Lotus is designed specifically for women and addresses health issues unique to women like perimenopause, menopause, hot flashes, painful periods, low back pain, swollen ankles, intense emotions, as well as uterine and breast tumors. This is achieved through a series of movements, divided into four routines, all featured on the DVD: 1. Shaking and cupping 2. Self-massage (of breasts and reproductive organs) 2. Vibrational sound healing 4. Kwan Yin closing.
The first series of movements starts by tapping the center of the chest. Lee describes this center biomedically as the thymus gland. Nüdan texts call it the “milk stream” (ruxi) and name it as the starting point of practice and as one of the main locations where the practice returns. The next movements include cupping the breasts, the neck, face, and abdomen, as well as the legs; special attention is given to breasts and ovaries, echoing nüdan materials. The second section describes a massage routine which includes, among others: ovarian, abdominal, groin, vaginal, kidneys, and breasts. All these areas are essential in nüdan practice. The movements, moreover, are performed nine times, which is also the typical number of repetitions in the nüdan tradition.
Daisy Lee uses biomedical language (thymus gland, ovaries, perimenopause, etc.) to talk about the locations as well as the effects of the practice, and she does not dwell on spiritual effects. However, the fact that she uses Tibetan vibrational sound healing as well as the Kwan Yin (Guanyin) closing, reflects the fact that spiritual practices have been integrated into a health routine. She does not say who developed the “Radiant Lotus” method nor does she discuss the mixing of Daoist (nüdan), Chinese Buddhist (Guanyin) and Tibetan Buddhist (sound healing) elements.
Both Lee and Liu Yafei speak of women’s yin nature and define it in a similar way to nüdan manuals, as soft, flowing, and internally beautiful. Both note that this nature may be more attuned to natural processes and therefore be better suited to accomplish a qigong routine. “There is a natural flow in a women’s body that helps in how you move in qigong. …you find that women are more naturally drawn to qigong” (Lee, Intro.). This is, not surprisingly, what nüdan texts already say, albeit in different terms, in the eighteenth century.
However, while Lee sees this as “a place of empowerment for women,” traditional texts use the “special predisposition of women” to maintain a woman’s place in society: in the home and away from the public eye; not a place of empowerment but a reiteration of the status quo. Both Liu Yafei’s and Daisy Lee’s instructional DVDs repeat many exercises and focus on locations featured in nüdan texts yet do not resemble each other very much. Both techniques, it appears, have a similar source, but have been refined and influenced by other traditions.
Mantak Chia


Mantak Chia was one of the first practitioners to bring neidan, or inner alchemy, to America in the 1970s. Since then, he has trained many Western practitioners to becoming full instructors while also publishing—in close cooperation with Michael Winn—a series of books that have strongly influenced the field of spiritual healing. Chia’s teachings have had a large impact on how Chinese healing and spiritual techniques are understood and adapted in the West. This is how he is described on many online sites selling his books:
A student of several Taoist masters, Mantak Chia founded the Universal Healing Tao System in 1979 and has taught and certified tens of thousands of students and instructors from all over the world. He is the director of the Tao Garden Integrative Medicine Health Spa and Resort training center in northern Thailand and the author of 31 books, including Fusion of the Five Elements, Cosmic Fusion, and the bestselling The Multi-Orgasmic Man.
In his many publications, Chia talks about inner alchemy and about the spiritual goals of the practice. His “Fusion of the Eight Psychic Channels: Opening and Sealing the Energy Body” describes the practice: “Advanced Inner Alchemy exercises that promote the free flow of energy throughout the body in preparation for the Practice of the Immortal Tao.” He credits several teachers for his knowledge of neidan practices, among whom Yi Yun “One Cloud Hermit” from Lone White Mountain, Cheng Yaolun and Pan Yu. However he does not give detailed explanation of their histories or of how the transmission of their knowledge (oral or written) to him took place. He does mention, however, that these teachers were already mixing elements from Daoism , Buddhism and Thai boxing in their teaching. To this knowledge, he added intensive study of Western medicine and anatomy.
Thus, while Chia’s publications make full use of the neidan ideology both in terminology and in the sequence of the practice, he also employs biomedical language. For example, ”When fully developed, the pineal gland becomes the compass that guides the spirit to the primeval Tao” (2005, 116). Differently from traditional neidan and nüdan manuals, he provides a profusion of details about the physical practices with many diagrams of the body, and especially of the genital area, and explains both practices and expected physical reactions in Western medical terms. Yet, he still describes the results in terms of transcendence, spirituality, and spiritual union. Thus Chia successfully maintains the esoteric nature and appeal of neidan while explaining its efficacy in a way that appeals to a Western audience.
In his Healing Love through the Tao (2005) on female practice, the technical language and description of the female body present several similarities to nüdan, starting with his use of language and the importance given to specific body locations: breasts and breast massages, ovaries, Governing and Conception Vessels (Dumai and Renmai)—all essential to female energy. He also presents an extensive discussion of sexual feelings; here is where his work differs significantly from traditional nüdan as well as from Liu Yafei’s and Daisy Lee’s modern take. Chia’s goal is to teach how to develop a better sexual relationship with a male partner through the strengthening of internal energy. Nüdan teachings, in contrast, acknowledge the emergence of sexual feelings during the practice, but teach the practitioner (who does not practice jointly with a partner) how not to dwell on them but sublimate them.
Last but not least, traditional nüdan texts talk at length about the practice of “Slaying the Red Dragon,” a technique of breast massage and internal visualization that results in the gradual disappearance of the menses. This is definitely not the message in Chia’s book.

“Slaying the Red Dragon” is the title of Chia’s video where , together with his wife Maneewan and one of their female practitioners, he describes their specific version of female practice. Despite the title, which is a clear reference to the traditional nüdan practice of eliminating the menstrual flow, the video does not discuss the disappearance of the menses. Instead, it focuses on “a Taoist way to control menstruation” attained through the strengthening of female sexual power with specific techniques like meditation, breast massage, vaginal massage, and the strengthening of the perineal muscles with external devices. In other words, the video pairs visualization techniques and breast massages from traditional nüdan, with sexual techniques that were never part of this traditionally solo technique to form an entirely new way of female sexual empowerment. Throughout video and book, Chia maintains a good balance between spirituality, sexuality, and health. The work remains a point of reference for all later books on neidan, qigong, and sexual health by other practitioners, providing a strong focus on exercises for pelvic floor health, ovarian and breast massage, and female sexual health. His work differs from other recent books on female qigong, which all give sound exercises for the female body—some for specific illnesses, others for specific life phases— in that the latter have few spiritual overtones.
Earth Qigong for Women
Tina Zhang starts her book in this way: “Earth Qigong is based on a special medical qigong developed and perfected over the course of 1,700 years by Daoists, Traditional Chinese medicine doctors, and qigong experts in China to address the needs of a woman’s unique anatomy” (2008, ix). She thereby equalizes Daoists, Chinese medical doctors, and qigong practitioners, mixing traditions and time periods into one unquestioned bundle. The term “Earth Qigong” and the Chinese subtitle to the book “Kungong”, which can be translated as “feminine practice,” are not explained. However, Zhang gives a general survey of the development of qigong and healing techniques in China, then focuses specifically on techniques for women. She says :
“This qigong program is designed to provide more movement than other qigong sets, some of which are based on seated meditation and do very little in motion. The basic goal of this program is to help women combat stiffness and the sedentary life that’s become too common. Its gentle approach helps women relax. Within this practice the deeper qi work will give positive energy to women, because it has the cultivation of the female center of qi as its main goal.” (2008, 48)
Zhang offers an apparently effective and comprehensive series of practices for women, called “The Earth Energy: Cultivating Female Energy,” “Creating Pelvic Health and Helping the Liver,” and “The Spirit of Vitality: Bringing out the Real Female Spirit.” These series focus on the pelvic area and on solving problems related to menstruation, breast swelling, and pre- and post-partum complications. Her sequences combine different styles of qigong while focusing on areas of specific female interest. She also discusses the importance of acupoints for women’s health, notably Meeting Yin at the perineum, Ocean of Qi (qihai) under the umbilicus, and Gate of Life (mingmen) between the kidneys in the back. She notes:
“Earth qigong includes several qi movements that exercise or massage the internal and external organs of the female body, some of which are not addressed in most other qigong routines or forms. These movement purposely move the blood and cultivate more of the female energy that women naturally have in their bodies in order to gain more inner power to ease and arrest uncomfortable symptoms during the different stages of menstruation, pregnancy, perimenopause and menopause.” (2008, 49). Zhang’s book betrays a deep knowledge of female physiology and offers good practical advice, but lacks historical perspective.
Women’s qigong For Health and Longevity
This book by Deborah Davis addresses women over forty and divides into sections according to age (40 to 49; 50 to 64; 65 and over). It, too, focuses on specifically female concerns like pre-menstrual syndrome, breast-health, depression, menopause, insomnia, osteoporisis, heart health, and sexual issues. Davis combines her extensive knowledge of both qigong and women’s health to produce a manual of general qigong exercises that are beneficial to a woman’s body. Unlike both traditional nüdan, Liu’s nüzi qigong and Chia’s guidelines, her practices focus less on specifically “female” areas of the body and instead devote practices to whole-body health. Still, even Davis acknowledges that the “Uterine Palace” (zigong) is fundamental in the female body, and has exercises called “Soothing the Middle”, “Renmai Massage” and “Pelvic Floor Lift” that focus on the middle of the body.
Qigong for Women

Dominique Ferraro, like Deborah Davis, uses her extensive knowledge of qigong and Chinese healing techniques, including her profound understanding of acupuncture, and applies it to the female body. The last two chapters of her book are devoted to “Qigong and Sexuality” and “Common Physical Problems of Women.” The chapter on sexuality introduces the concept of a healthy sexuality between men and women, recalling the tradition of Chinese sexual manuals; it refers directly to Mantak Chia’s work, then notes the importance of blood and its proper flow. The chapter on common ailments concentrates on bones, joints, teeth, memory, and hearing; only at the end does it turn to more specific gynecological problems and pregnancy. Again, this is a good manual for general health, but the advice is often not specific to women. As Davis’s work, her book is eminently interested in physical sequences and effects.
A Woman’s Qigong Guide

This book by Yangling Lee Johnson (2001), as noted in the title, is not only about qigong but also about movement, diet, and herbs—albeit within the Chinese tradition. It provides a fairly long historical introduction about the development of Chinese medicine and qigong. The introduction also includes a personal perspective, and Johnson shares her story of self-healing during the Cultural Revolution and the hardship she underwent when relocating to the U.S.
Unlike other books of this kind, this work does not consist largely of detailed descriptions of practice postures. Only in Chapter 5 does Johnson begin to talk about “short forms,” i.e., quick postures to do in the morning, in the car, at work, outside, etc. These quick forms deal with problems such as sterility, depression, weight loss, the flu, amenorrhea, and the like. Johnson’s book contains various passages she herself translates from Daoist and Chinese medical texts, scattering advice about almost everything: alcohol intake, work, nails, sexual activity, sleeping, sweating, dieting, and more. The book concentrate on the physiology of women or on specific areas of the female body. In sum, it is not quite a qigong guide for women as advertised in the title, but rather a general guide on wellbeing for women that mixes psychological, dietary, and energetic advice.
Conclusion
In sum, I find that the field of women’s qigong publications in Western Languages is developing fast, and at the same time has a lot of room to grow. Some of the above publications are just beginning to discuss what it means to practice neidan and qigong as a woman, what are the important areas to concentrate on, and where the practice should take us. In most of the publications reviewed, there is particular attention to female physiology and to ailments that are specific to women, and there are a variety of techniques offered to relieve them. Some concentrate on health, other on sexuality, others again mix healing, sexuality and spirituality. Some are more thorough than others, but all of them, to a certain extent, lack historical perspective. Though I realize that not all are meant to include historical introductions to the field, paying attention to the historical significance and development of a tradition, as well as describing one’s affiliations with contemporary masters, and one’s place in that tradition, puts the physical practice in a clearer context. My interest in this review was to highlight the appropriation and adaptation of a Chinese tradition with roots in a religious practice. Pointedly, most if not all of the above publications do not portray women’s practices in any way as religious.
References
Barnes, Linda. 1998. “The psychologyzing of Chinese Healing Practices in the United States”, Culture, Medicine and Psychiatry 22: 413–443
Chen, Nancy N. 2003. Breathing Spaces: Qigong, Psychiatry, and Healing in China. New York: Columbia University Press.
Cohen, Michael. 2002-03. “Healing at the Borderland of Medicine and Religion: Regulating Potential Abuse of Authority by Spiritual Healers.” Journal of Law and Religion, 18.2
Kohn, Livia, and Robin R. Wang. 2009. Internal Alchemy: Self, Society, and the Quest for Immortality. Magdalena, NM: Three Pines Press.
Ots, Thomas. 1994. “The Silenced Body—the Expressive Leib: On the Dialictic of Mind and Life in Chinese Cathartic Healing.” In Embodiment and Experience: The Existential Ground of Culture and Self, edited by Thomas J. Csordas. Cambridge: Cambridge University Press.
Palmer, David. 2007. Qigong Fever: Body, Science and Utopia in China. New York: Columbia University Press.
Valussi, Elena. 2003. “Beheading the Red Dragon: A History of Female Inner Alchemy in China.” Ph. D. Diss., School of Oriental and African Studies, University of London, London.
Valussi, Elena. 2008a. “Female Alchemy and Paratext: How to Read Nüdan in a Historical Context.” Asia Major 21.2.
Valussi, Elena. 2008b. “Blood, Tigers, Dragons. The Physiology of Transcendence for Women.” Asian Medicine: Tradition and Modernity 4.1.
Valussi, Elena. 2008c. “Men and Women in He Longxiang’s Nüdan hebian (Collection of Female Alchemy).” Nannü: Men, Women and Gender in Early and Imperial China 10.2.
Valussi, Elena. 2009. “Female Alchemy: An Introduction.” In Internal Alchemy: Self, Society, and the Quest for Immortality, edited by Livia Kohn and Robin R. Wang, 142-64. Magdalena, NM: Three Pines Press.
Winn, Micheal, 2009. “Daoist Internal Alchemy in the West”. In Internal Alchemy: Self, Society, and the Quest for Immortality, edited by Livia Kohn and Robin R. Wang, 142-64. Magdalena, NM: Three Pines Press.
Xun, Liu, 2009, Daoist Modern; Innovation, Lay Practice and the Community of Inner Alchemy in Republican Shanghai, Cambridge and London, Harvard University Asia Center, Harvard University Press